Claims organizations across the insurance industry are experiencing unprecedented operational pressure thanks to the sheer volume of claims — fueled by climate-driven losses, inflationary cost pressures and evolving loss patterns.
These have all created a complex environment for claims executives, operations leaders and chief data officers to navigate.
Customers expect the same level of service and immediacy they get in ecommerce or digital banking, regardless of your workload. For chief customer officers and operational teams, this sets a new minimum standard: fast, transparent and proactive communication throughout the entire claims lifecycle.
In addition to increased customer expectations, regulators have also raised the bar around fair outcomes, clear documentation and evidence-backed decision-making, adding pressure to those overseeing compliance risk and operational consistency.
According to McKinsey’s Global Insurance Report 2025: The Pursuit of Growth, insurers leading in claims transformation are those strengthening data foundations and redesigning feedback loops to support faster, more transparent claims outcomes.
McKinsey’s report emphasizes a truth every claims leader already knows:
Claims processing is only as fast as the data behind it. That data is more often than not inconsistent and not trustworthy.
The hidden bottleneck in claims: Untrusted, inconsistent and unstructured data
Even in mature insurance organizations, the claims journey relies heavily on information flowing from an expansive ecosystem of different tools and partners — from policy administration and underwriting to broker portals, contact centers and repair networks to medical providers and third-party data services.
Each contributes critical information, but very few (if any) align on consistent data definitions and structures. The problem with this is that it creates systematic friction, including:
- Multiple versions of customer records, claimants and policies. There’s no single, authoritative source of truth, so adjusters have to spend more time reconciling conflicting versions.
- Coverage and product definitions that vary by system or region. Deductibles, exclusions and benefit logic get misaligned across platforms, creating inconsistencies.
- Unstructured documents that lack metadata. Photos, invoices, medical reports and legal correspondence often arrive without consistent tagging, which slows down digital workflows.
- Third-party data that arrives in conflicting formats. Repair shops, medical providers and external partners typically send information in different formats that require timely manual translation.
- Fragmented reference data. Cause of loss codes, provider categories and document classifications vary across teams, creating confusion and exceptions.
Deloitte’s 2025 Global Insurance Outlook report confirms that improving data governance and transparency is a top operational priority for insurers, who need to balance efficiency, regulatory pressure and rising loss costs.
Why digital claims automation fails without trustworthy data
Many chief information officers and claims transformation leaders have invested heavily in automated platforms, rules engines and AI to accelerate the claims journey. Yet automation often stalls as a result of downstream systems that can’t interpret inconsistent or incomplete data.
This shows up in a few core stages of the claims process:
- First Notice of Loss (FNOL). When customer and policy details are duplicated or outdated, automation can’t correctly pre-fill or validate core fields, leading to higher abandonment and frustration.
- Triage and routing. Triage engines rely on structured attributes, like severity, coverage and claimant details. When these differ across systems, rules misfire and claims get routed incorrectly.
- Fraud detection and risk evaluation. Special investigative units (SIUs) rely on accurate identity and entity relationships, but a poor data structure weakens fraud signals and risk models.
- Straight-through processing (STP). If you don’t standardize benefit rules and entitlements, STP fails, pushing claims back into manual queues.
EY’s 2025 Global Insurance Outlook: Driving growth through advanced technology and data capabilities notes that manual interventions will remain common in automated claims flows due to inconsistencies in underlying data.
Automation hasn’t failed — it has revealed where data isn’t ready for automation.

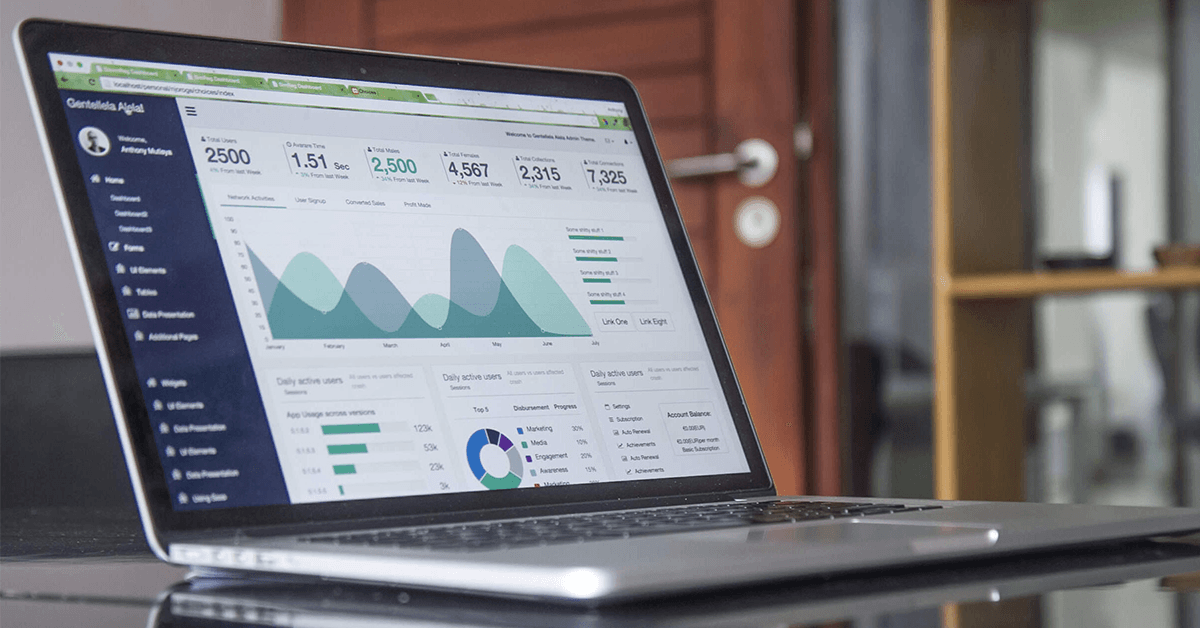
Rebuilding claims for speed: A data-driven operating model
Leading insurers have pivoted away from process-only transformation. They’ve embraced a model that places trustworthy data at the center of claims operations. This shift has resonated strongly with C-suite leaders responsible for supporting both short- and long-term operational goals and resilience.
This modern, data-driven claims operating model includes the following:
Clear, consistent claims entities
A shared, authoritative model of customers, claimants, beneficiaries, providers and assets that immediately simplifies integration and automation.
Governed policy, product and entitlement structures
You must consistently define and version coverage logic, benefits, deductibles and exclusions. This enables claims directors and ops leaders to deliver predictable decisions.
Reliable identity resolution
When you automatically match and deduplicate customer and claimant identities, SIU teams get clearer visibility, and automation engines gain accuracy.
Standardized metadata for risk, fraud and regulatory needs
Standardized metadata is an absolute must-have for compliance teams and regulatory reporting groups.
Harmonized reference data across teams and geographies
Data that’s aligned across teams and geographies is a key requirement for service consistency across branches, regions and distribution partners.
End-to-end lineage and auditability
This is critical for CIOs, CDOs and governance teams that must demonstrate data confidence to regulators.
According to KPMG’s 2025 Insurance transformation: The new agenda, unstructured or poor-quality data prevents insurance organizations from identifying inefficiencies and making informed decisions.
Claims leaders are increasingly focused on foundational data alignment — not just workflow optimization.
What trustworthy data enables across the claims journey
With trustworthy data in place, claims leaders, SIU teams and ops managers can see gradual improvements across every stage.
A smoother FNOL
Clean, unified policy and customer data reduces rework and immediately improves customer perception.
Faster, more accurate triage
Coverage- and severity-based routing work as intended, and STP rates rise.
Higher investigation efficiency
Adjusters spend less time resolving conflicts and more time progressing the claim.
Fairer, more consistent settlement decisions
Governed entitlement logic ensures similar claims result in similar outcomes.
Reduced leakage and stronger recovery
More accurate data yields stronger subrogation and salvage identification.
Simpler regulatory reporting and audit readiness
Lineage and consistent data structures make compliance far easier.

The competitive advantage of data-driven claims operations
Trustworthy data is both an operational necessity and competitive advantage in a few ways, including:
- Faster resolution and increased customer satisfaction resulting from reduced friction that creates a better claims experience and boosts retention.
- Increased operational efficiency from less manual work, fewer exceptions and smoother digital journeys.
- Enhanced fraud and risk controls as a result of identity and metadata clarity that significantly strengthen SIU capabilities.
- Improved loss ratios thanks to fewer overpayments, better recovery and reduced disputes.
- Stronger regulatory resilience from reliable lineage and governance that reduce compliance exposure.
According to Carmatec, trusted, well-structured data is the foundation of analytics-driven claims transformation and performance improvement.
The insurers of the future win with trustworthy data
Whether it’s claims, fraud, customer experience or operations, they all depend on a reliable foundation of trustworthy data. One that allows for speed, fairness, transparency and efficiency. That’s why insurers are investing in strong data foundations.
When everything’s powered by trusted data, automation becomes reliable — not fragile. Handlers gain clarity, customers experience confidence instead of frustration and regulators get much-needed transparency.
The insurers shaping the future of the industry are those prioritizing consistent and governed data as a central strategic capability vs. an afterthought. They’re using trustworthy data to deliver faster settlements, stronger customer outcomes, and more resilient operations.